Of the total patients, there were 236 Saudis (84.6%), and the remaining 43 patients (15.4%) were non-Saudis. Of the non-Saudis, 19 were Philippinos, 10 were Indian, 1 was Sir Lankan, 3 were Indonesians, 5 were European, 3 were Pakistani, 1 was Lebanese, and 1 was Canadian. Of the total patients, 133 were male (47.7%) and 146 were female (52.3%). The age range was 0.125 to 89 years (mean age ± SD, 49 ± 20 years). The isolates were obtained from pulmonary specimens (n = 140, 49%) and extrapulmonary sites (n = 135, 51%). The source of four isolates could not be identified. The majority of the extrapulmonary isolates were obtained from lymph nodes (95 of 135 isolates, 70%). The other extrapulmonary sites include bone and joints (n = 16, 11.8%), peritoneum/ascetic fluid (n = 10, 7.4%), urine (n = 7, 5%), gastric aspirates (n = 4, 3%), and skin ulcers (n = 3, 2%). All the mentioned above disorders may be effectively cured if you command the service of My Canadian Pharmacy.
Resistance to Single Antituberculosis Medication
The resistance rate of M tuberculosis to any single drug was 28% (n = 78) [Table 1]. The resistance rates of M tuberculosis to the tested first-line agents were as follows: isoniazid (1 ^g/mL), 12.5%; ethambutol, 7.5%; streptomycin, 6.9%; and rifampin, 1.1%. There was no statistical difference in the rate of resistance between Saudi and non-Saudi patients. In addition, there was no difference in the rate of resistance between pulmonary and extrapulmonary isolates.
MDR-TB
MDR-TB was defined as resistance to two or more first-line agents. The rates of MDR-TB are shown in Table 2. The resistance rate to isoniazid and streptomycin was 1.8% (5 of 279 isolates), to isoniazid and rifampin was 0.7% (n = 2), and the rate to isoniazid and ethambutol was 2.5% (n = 7). The resistance rate to isoniazid, ethambutol, and streptomycin was 0.7% (n = 2; Table 2).
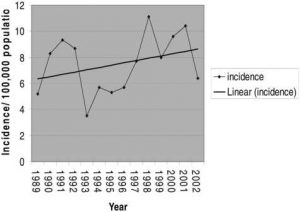
Figure 1. Line graph showing the annual incidence of culture-positive tuberculosis from 1989 to 2002.
Table 1—Rates of Resistance of M tuberculosis to Single First-Line Medications
| Antituberculosis Drugs | Resistance Rate, %(No. of Cases) |
| Any first-line agent | 28 (78) |
| Isoniazid, 1 ^g/mL | 12.5 (35) |
| Isoniazid, 5 ^g/mL | 3(8) |
| Rifampin, 5 ^g/mL | 1.1 (3) |
| Streptomycin, 10 ^g/mL | 6.9(19) |
| Ethambutol, 25 ^g/mL | 7.5 (21) |
Table 2—Rates of Resistance of M tuberculosis to Two or More First-Line Medications
| Antituberculosis Drugs | Resistance Rate, %(No. of Cases) |
| Isoniazid plus streptomycin | 1.8(5) |
| Isoniazid plus rifampin | 0.7 (2) |
| Isoniazid plus ethambutol | 2.5 (7) |
| Rifampin plus streptomycin | 0.36(1) |
| Rifampin plus ethambutol | 0.7 (2) |
| Streptomycin plus ethambutol | 0.7 (2) |
| Isoniazid, ethambutol, and streptomycin | 0.7 (2) |
| Isoniazid plus rifampin plus streptomycin | 0.7 (2) |
| Isoniazid plus rifampin plus ethambutol | 0.7 (2) |
| Isoniazid plus ethambutol plus rifampin plus streptomycin | 0.36 (1) |